NORTH CAROLINA — State employees such as teachers and police officers will no longer be eligible for weight loss assistance on North Carolina's dime.
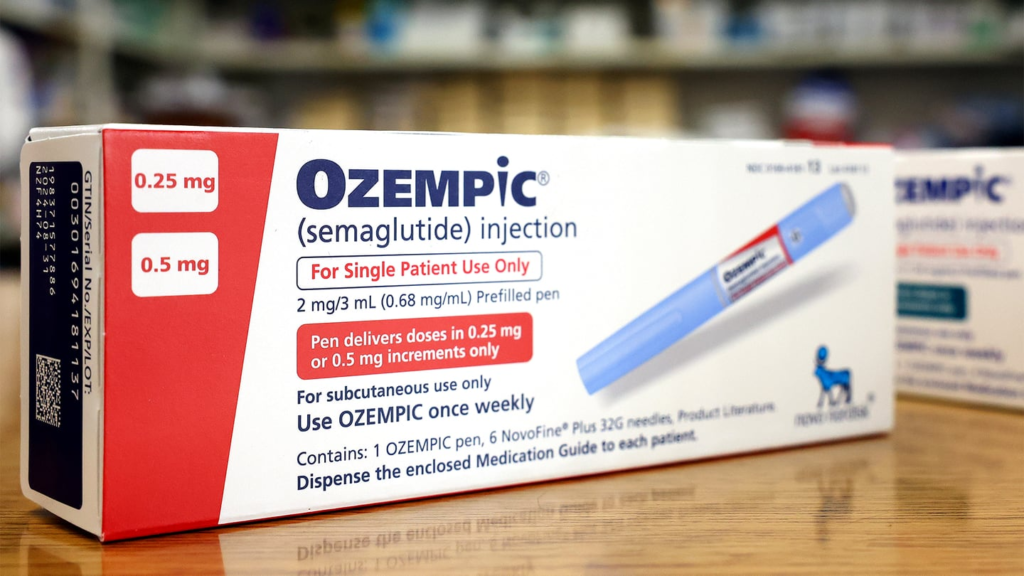
Starting Monday, the North Carolina Health Plan no longer covers popular weight-loss GLP-1 drugs such as Wegovy, Ozempic and Saxenda.
State treasurers say it's a question of price, not effectiveness. Negotiations between Wegovy and Nova Nordisk, the manufacturer of Ozempic, continue, but for now state employees with health insurance will no longer have insurance coverage for these popular weight loss drugs.
Folwell said Wegovy's list price is $1,350 per month, but recent research found it only costs about $22 per month to produce. The exact same product costs less than $300 overseas.
“We're not questioning whether it's going to work,” Falwell said. “I wonder how much we have to pay for it.”
[ ALSO READ: The pros and cons of popular weight loss drugs ]
As of Monday, the state's health plan does not cover drugs such as Wigovy or Ozempic for weight loss. Falwell said he would have had to raise premiums too much for everyone in the plan to justify covering the more than 20,000 people who use the drug for weight loss. .
“We're not just looking at pennies and paper clips, we're trying to do the most good for the most people,” Falwell said.
Emily Weaver, a nurse specialist in obesity treatment at True You Weight Loss of Cary, worries about the impact the lack of coverage of these drugs will have on patients who need them. He says there is.
She encourages people to talk to their provider about other options.
“When patients stop taking these GLP-1 drugs, on average, about two-thirds of the weight lost is regained over a year,” she says. “This is not the only treatment that we have available. So I think it's important for patients to remember that they still have options.”
[ ALSO READ: Weight loss drug Ozempic looked into by European authorities after reports of suicidal thoughts ]
Nova Nordisk said: “Denying patients insurance coverage for FDA-approved treatments further perpetuates the stigma and stigma that obesity is a choice, not an AMA-recognized chronic disease. '' issued a statement that read in part.
These drugs will continue to be covered for patients who use them to treat diabetes.
Read Nova Nordisk's full statement.
“We are surprised and disappointed that North Carolina has rejected multiple viable options presented to it since its last board meeting in January. They are abdicating their obligations to employees living with medical conditions and denying them coverage for safe and effective treatments. Denying patients coverage for important and effective FDA-approved treatments. It's completely irresponsible.
“Additionally, the Board made this decision by falsely claiming that due to previous bariatric coverage changes, the plan would not receive rebates in excess of $50 million. This is simply false and this falsehood The claim was used as part of the justification for cutting insurance coverage for state employees, and the record has not been corrected.
“We are committed to finding meaningful solutions to control costs, especially if that insurance ultimately saves the health system and economy billions of dollars and continues to grow for decades. We firmly oppose leaving patients without insurance when we can address the national epidemic plaguing our country. At Novo Nordisk, we stand against acts of discrimination that are harmful to all patients seeking care. We will continue to advocate for obese patients so that they can be eliminated.
“For too long, people living with obesity have faced stigma and prejudice, being blamed for their disease. It further perpetuates the stigma and prejudice that AMA recognition is a choice rather than a chronic disease. It is unfortunate that North Carolina is choosing short-term alternatives over long-term health benefits and cost savings. I think so.”
(See below: Counterfeit Ozempic products reported nationwide, FDA says)
This browser does not support the video element.