Written by Jamie Baxley
When North Carolina began expanding Medicaid on Dec. 1, state officials said the measure would provide health insurance to an estimated 600,000 low-income adults over two years.
It took just two months to reach 58% of that goal. More than 346,400 newly eligible people were approved for coverage as of Feb. 1, according to data from the North Carolina Department of Health and Human Services.
The rapid pace of enrollment was one of several expansion-related success stories DHHS leaders shared with lawmakers during last week's meeting of the monthly Joint Legislative Oversight Committee on Medicaid. This was the first formal report the department submitted to the 14-member committee since the expansion took effect.
The expansion raised state income limits for Medicaid and expanded eligibility to people with annual incomes up to 138 percent of the federal poverty level ($25,820 for a family of three) based on household size. The previous limit was 100%.
Jay Ludlum, the state's deputy secretary for Medicaid, told the committee that DHHS has undertaken the expansion “in a member-focused manner.” About 273,000 adults enrolled in Family Planning Medicaid, a limited coverage program for reproductive health services, were automatically upgraded to full Medicaid coverage when the expansion began in December.
“We ran an algorithm based on the information we had about that population,” Ludlum said. “We determined which individuals were eligible for Medicaid expansion and who were not, and we moved those individuals who were eligible. [did] Qualify for expansion. ”
He said this strategy has helped the department get back on track. Most new beneficiaries obtained Medicaid with little or no action required on their part.
“These people didn't have to go to the office,” Ludlum said. “We didn't have to call a DSS worker. We didn't have to fill out any forms. In effect, they woke up on his December 1st with a card in his hand and access to full Medicaid benefits from day one.” It is now possible.”

People who did not participate in the first wave of automatic enrollment have steadily enrolled in Medicaid since the expansion began. Ludlum said DHHS is adding an average of 1,000 beneficiaries to its roster each day, but he believes that number will decrease in the coming weeks.
A disproportionate share of the state's new enrollees are residents of economically disadvantaged counties. That's not entirely surprising, according to Ludlum. He said the expansion is expected to have a significant impact on rural areas.
“Broadly speaking, we expected high enrollment numbers in some of these communities,” he said. “These are areas where individuals potentially hold multiple jobs to make a living.”
“Knocking on death's door”
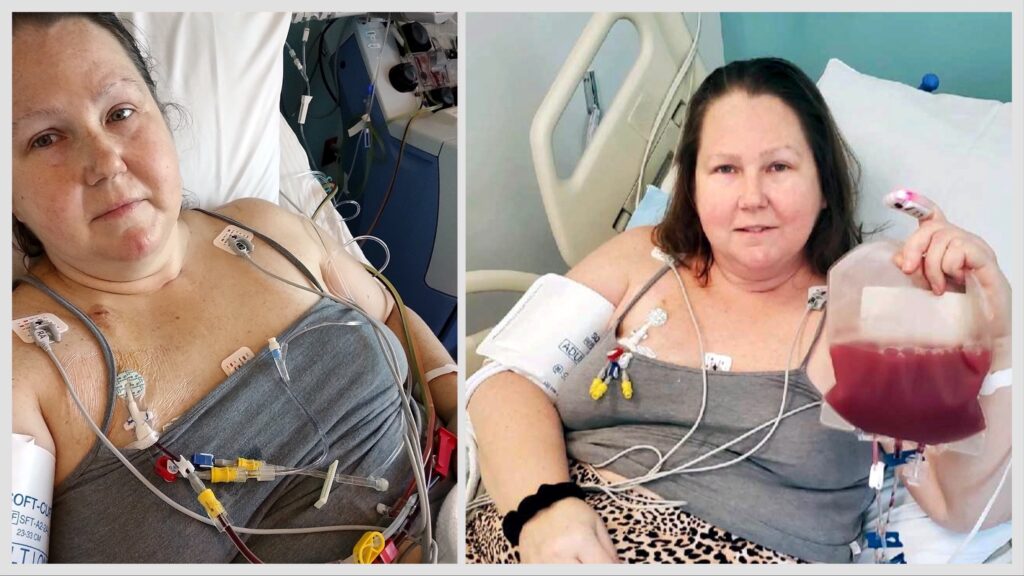
For people like Deanna Brandon, the value of Medicaid can be measured in days, not dollars.
A Rowan County resident diagnosed with a rare blood cancer in 2022 was given less than three years to live unless he receives a stem cell transplant. Brandon, whose story was first reported by NC Health News, couldn't afford the expensive surgery without health insurance. And her biological opportunities were becoming increasingly narrow.
The chemotherapy that helped manage Brandon's cancer symptoms could have irreversibly damaged her cells and compromised the effectiveness of the transplant. Due in part to the physical strain of her treatment, she is no longer able to work.
Brandon believed his plight made him eligible for Medicaid. After all, cancer was technically an obstacle preventing her from earning a steady income. But when she applied for insurance last year, before the expansion went into effect, she was told her condition didn't meet the state's eligibility requirements.
She became hopeful when Gov. Roy Cooper signed the expansion into law last March. With her new income threshold, Brandon will qualify for Medicaid regardless of her ability to work.
Her hopes turned to disappointment as protracted General Assembly disputes over the state budget delayed implementation of the expansion. Lawmakers ultimately agreed to advance the spending plan in September and begin the expansion in December, months later than planned.
By then, Brandon had successfully appealed the state's decision to deny his Medicaid application. She was approved for coverage just before the expansion went into effect.
On Tuesday, she completed the first of two procedures to harvest stem cells from her blood at Novant Health Presbyterian Medical Center in Charlotte. The cells are scheduled to be transplanted into her body on March 1st.
Brandon said his immune system would be “completely wiped out” after the surgery and he would be forced to isolate at home for three months.
“I can't go anywhere except for doctor's appointments and no one can come see me except my only caregiver,” she said. “I will be like a newborn baby. Over the next two years, I will have to retake all the vaccinations I received as a child.”
Still, Brandon believes this ordeal is a small price to pay to spend more time with loved ones. Her transplant is expected to extend her life by about 10 years.
“I don't want to say that without Medicaid I was knocking on death's door, but that's what my doctor told me,” she said. “Ten years may not seem like a long time to many people, but when you're faced with just three years, 10 years sounds great.”
Is it possible that NC will lead the way?
Lawmakers in Florida, one of 10 states that have yet to expand Medicaid, may now be looking to North Carolina as a model.
Sen. Kevin Corbin, a Macon County Republican who serves on the oversight committee, traveled to Tallahassee this week to discuss North Carolina's experience with Florida lawmakers. Mr Corbyn said the talks went “very well”.
“As their new leadership prepares to take office after elections next year, I don't think anyone is going to say they're going to do this or that yet,” he said in a phone interview Wednesday. said. “But I think they're definitely encouraged by what I've talked about and I think they're willing to consider what we did in North Carolina.”
After the Affordable Care Act took effect in 2012, health care advocates began pushing for North Carolina to expand access to Medicaid, but their efforts were repeatedly blocked by Republicans in Congress. Last year's promise of more than $1.6 billion in federal financial incentives prompted the state's Republican leadership to reconsider and allowed the expansion to pass with bipartisan support.
Corbin, a longtime insurance agent, said Medicaid is “cheaper than private insurance or Medicare” for North Carolina. The program, which serves about 3 million participants in the state, costs about $21 billion to operate, most of it covered by the federal government and hospitals.
Corbyn said the state would be paying “just over $100 per month per legislator.”
Expansion would mean more North Carolinians receiving Medicaid, but federal incentives would ease the state's financial burden. Mark Collins, a fiscal analyst for the North Carolina General Assembly, told the oversight committee that the state's overall share of program costs is expected to drop by nearly 15%.