To our knowledge, this is the first study to investigate factors influencing distributed practice psychiatrists' willingness to engage in educational activities, a crucial factor for the growth of DME. Actively involve local psychiatrists in this transformation process, while also providing academic decision-makers with evidence-based findings that can contribute to making informed decisions about the expansion of DME. provided to you.
As a result, among psychiatrists, clinical training/supervision of psychiatry residents, delivery of lectures, skills-based instruction/examination, and training/supervision of Canadian and internationally trained psychiatry fellows. It became clear that there was a strong desire to participate in various educational activities, such as providing educational services. The average positive response rate achieved in our study (81.98%) significantly exceeded the participation rate of specialists in educational activities (65%) according to the 2004 CFPC/CMA/RCPSC National Physician Survey . [13]. Interestingly, this enthusiasm continues despite the fact that the majority have no formal training in medical education. This finding challenges the traditional definition of a clinician-educator by the Royal College of Canada, which typically includes formal education in education. [14]. It combines expertise with the principles of responsibility, selflessness, and wisdom, and emphasizes physicians' unique dedication to serving their clients and society. [15]. However, despite these encouraging results, challenges remain. This study identified significant barriers that prevent psychiatrists from actively participating in educational activities. The biggest barriers reported were lack of protected time for education/training and inadequate financial incentives. Interestingly, these findings paradoxically resonate with the existing literature. However, these studies highlight the well-documented struggles that physicians face in balancing clinical practice and academic studies. [16,17,18,19,20]. On the other hand, there are commonly recognized problems such as lack of awareness, inadequate teacher training, unmotivated students, low interest in teaching, bureaucratic school culture, and suboptimal learning environments. Deviating from the barrier. [21].
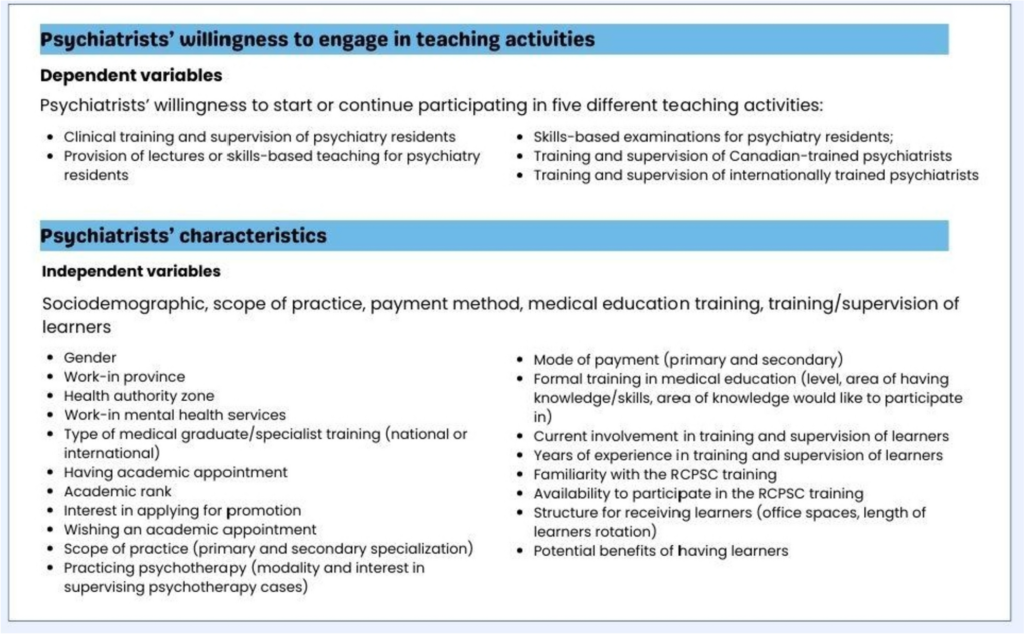
However, the study's most interesting findings lie in the factors associated with and that can predict psychiatrists' motivation to educate. The main factor associated with psychiatrists' willingness to participate in the five specific educational activities investigated in this study was the availability of RCPSC/CBD training. This training was conducted by the RCPSC to transform graduate medical education in Canada. CBD focuses on achieving competencies rather than traditional time-based training and emphasizes outcomes such as the ability to apply medical knowledge, professionalism, communication, and collaboration skills. [22].
The relationship between RCPSC/CBD training and clinicians' willingness to participate in educational activities may be multidimensional but has not yet been reported in the literature. Nevertheless, individuals expressing interest in such training prefer modern educational approaches that emphasize practical skills and competency development, and show an initial tendency to increase their participation in educational activities. There may be. Training psychiatrists with the necessary experience to continue providing outreach services in rural practice is one strategy to address the needs of underserved areas from an educational perspective . [23]. This result may highlight the potential knock-on effects of participating in a structured training program, even if lack of training was not considered a significant barrier for participants to engage in educational activities. there is.
Availability of RCPSC/CBD training is the only indicator of psychiatrists' willingness to participate in four of the five educational activities, except for involvement in the training/supervision of internationally trained psychiatrists. emerged as a predictive factor. This finding provides an easy and reliable method to identify psychiatrists in her DME facility who are likely to contribute to educational activities.
Other variables were found to be associated with psychiatrists' willingness to participate in educational activities. Psychiatrists working in New Brunswick participated more actively in these activities compared to psychiatrists in Nova Scotia. This finding suggests that the motivations and opportunities for psychiatrists to contribute to medical education may vary by region. This finding supports the local need to expand the number of psychiatrists in the New Brunswick region.
Academic commitment to Dalhousie University's Department of Psychiatry was also significantly associated with willingness to participate in providing lectures and skills-based education to psychiatry residents. This finding once again revealed the association between academic affiliations on physicians' involvement in medical education. Psychiatrists with academic appointments often have access to resources, mentorship, and a supportive academic environment, which may foster enthusiasm for teaching and supervisory activities.
Psychotherapeutic practice also emerged as an important factor related to psychiatrists' willingness to engage in the provision of lectures and skills-based education to psychiatry residents. Psychiatrists who specialize in psychotherapy often develop strong interpersonal and communication skills, which are highly transferable to teaching and coaching roles. These skills include active listening, empathy, and creating a supportive and collaborative therapeutic environment. In this context, the willingness of these psychiatrists to engage in educational and mentoring activities may be due to their special skills.
In addition to considering the willingness of psychiatrists to engage in educational activities, it is important to consider other factors that may influence the success of DME expansion.Previous research has shown that early exposure to the field of psychiatry is correlated with later practice in rural and remote areas. [24]. Future research could examine how expanded DME residency training and academic education opportunities influence this decision for future generations of medical students.