On January 9, 2024, the Centers forMedicare and Medicaid Services (CMS) approved New York’s request to amend its Medicaid section 1115 demonstration waiver, “Medicaid Redesign Team.”1 New York State announced that the approved “health equity waiver amendment” would provide $7.5 billion over three-and-a-half years to support the State’s efforts to advance health equity, reduce health disparities, support the delivery of health-related social needs (HRSN) services, and promote workforce development.2
New York joins a growing number of states receiving CMS authorization and funding for services that address HRSN and the infrastructure to deliver HRSN services, and their funding level of over $3 billion is the highest CMS has approved to-date. Also, notably, CMS has authorized funding to establish a statewide entity focused on advancing health equity, bolstering financially distressed safety net hospitals through the creation of global budgets, and strengthening the health care workforce.
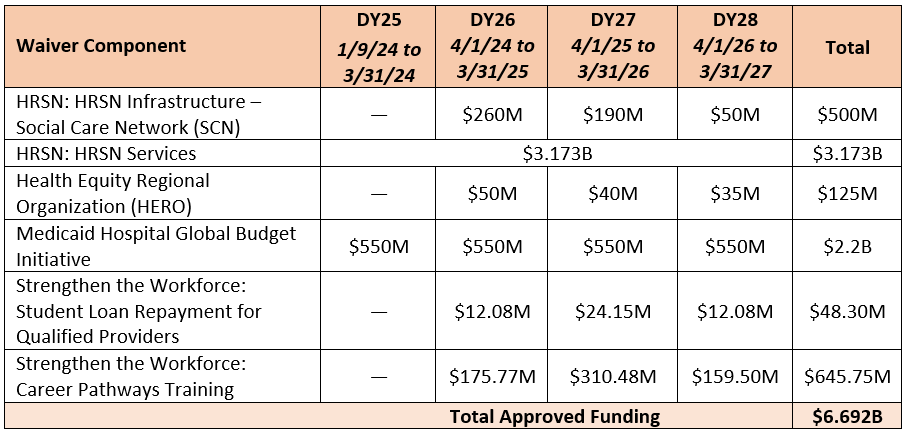
CMS authorized $6.69 billion in investments for these initiatives and others (see Table 1 below) for the approximately three-year waiver period from January 9, 2024, through March 31, 2027 (the remaining term of the Section 1115 Medicaid Redesign Team waiver).
As a condition of the approval, CMS is requiring New York to increase Medicaid provider payment rates for primary care, behavioral health, and obstetrics care if their Medicaid payment rate is below 80% of Medicare rates in any of these three categories. In addition, even if none of these Medicaid rates are below 80% of Medicare rates, New York is required to invest approximately $199 million in provider payment rate increases as part of the amendment. This is consistent with CMS’s HRSN guidance and the Special Terms and Conditions (STCs) of other state waivers that include HRSN initiatives.
Table 1. Funding Distribution in Approved Waiver Amendment
Health-Related Social Needs (HRSN)
New York’s 1115 waiver approval authorizes the largest funding to-date for the State to pay for services that address HRSN and support the infrastructure needs of the entities that will connect Medicaid members to these services.
HRSN Services
CMS authorizes $3.173 billion to provide increased coverage of certain services that address HRSN, including:
- Housing supports;
- Pre-tenancy services;
- Tenancy sustaining services;
- Housing transition navigation services;
- Nutrition supports;
- Case management; and
- Transportation for members to covered HRSN services and case management activities.
HRSN Infrastructure
CMS also authorizes $500 million for New York to establish Social Care Networks (SCNs)—contracted entities in each of the State’s nine regions that will provide HRSN screening and referral services to otherwise eligible Medicaid beneficiaries who are targeted populations for HRSN services. This new funding can be used for technology; development of business or operational practices; workforce development; and outreach, education, and stakeholder convening. Since waiver approval, New York has already issued a request for applications for entities interested in becoming SCNs.
HRSN Services Delivery and Payment
HRSN services will be delivered by HRSN service providers in collaboration with SCNs. SCNs will be required to establish a network of providers and ensure the HRSN service providers have sufficient experience and training in the provision of the offered HRSN services. Medicaid managed care plans will contract with SCNs to deliver the HRSN services and use rates set by the State to pay for HRSN services.
Health Equity Regional Organization (HERO)
CMS provides up to $125 million to New York State to establish a HERO, a single, statewide entity that will be tasked with designing and developing regionally-focused approaches to reduce health disparities, advance health equity, and support the delivery of HRSN services. The HERO will be a unique model for New York, serving in an independent administrative, policy design, and coordination role to support service delivery. The HERO will conduct the following five activities: data aggregation, regional needs assessment and planning, recommendations development and program analysis.
Medicaid Hospital Global Budget Initiative
CMS provides up to $2.2 billion to support the transition of select financially distressed hospitals to global budgets to enable hospitals to focus on population health and health equity, improve quality of care, stabilize safety net hospital finances, and advance accountability.
Workforce
CMS authorizes up to $694 million to support workforce recruitment and retention to promote the increased availability of certain health care practitioners who serve Medicaid members. New York will implement two workforce initiatives: Student Loan Repayment for Qualified Providers and the Career Pathways Training (CPT) Program.
Student Loan Repayment for Qualified Providers
New York will support repayment of student loans for providers who make a four-year full-time commitment to serving at least 30% Medicaid and/or uninsured members. Providers who are eligible for the student loan repayment program include psychiatrists, primary care physicians, and nurse practitioners, with an emphasis on providers serving children and youth.
Career Pathways Training (CPT) Program
The CPT program is designed to build up the allied health and other health care workforce by funding training and education that focus on career advancement and unemployed individuals. There is a pipeline for career advancement for individuals within the health care field, as well as pipeline for job-seeking individuals who want to enter the field.
Provider Rate Increases
As a condition of approval for certain authorities under the waiver, CMS requires the State to increase Medicaid fee-for-service provider base payment rates and Medicaid managed care payment rates in primary care, behavioral health, and obstetrics care by at least two percentage points if New York’s Medicaid-to-Medicare provider rate ratio is below 80% of Medicare rates in any of these three categories.
Applying the analysis from peer reviewed journal articles, New York’s Medicaid fee-for-service physician fees are lower than the national average for primary care, obstetrics care, and behavioral health. Medicaid fee-for-service physician fees are at:
The State is also required to invest approximately $199 million in rate increases as part of the amendment, which must be sustained by the State once implemented.
IMD Transformation Demonstration Program
CMS approves the SUD component of New York’s IMD Transformation Demonstration Program amendment request, providing New York with SUD demonstration authority to receive federal Medicaid matching funds for services delivered to beneficiaries residing in an institution for mental diseases (IMD) with a SUD diagnosis.3The State will be eligible to receive federal match for Medicaid beneficiaries who are short-term residents in IMDs for coverage of medical assistance, including OUD/SUD services.
Requests Not Approved at This Time and Future Requests
Notably, New York’s envisioned advanced value-based payment (VBP) models proposal4—which comprised $6.7 billion, or half of the total requested amendment funding—is excluded from the approved waiver amendment. The State envisioned making financial incentives available to Medicaid managed care plans and providers that met State-set criteria for health-equity focused VBP contracts, with some structured as global prepayment arrangements. The approved waiver amendment excludes this proposal entirely; while CMS references New York’s goal to make “significant movement” towards VBP strategies by the end of the demonstration, advanced VBP contract related activities are contained to the HERO’s responsibilities to make recommendations on how the State can incorporate HRSN into VBP methodologies.
SMI Component of IMD Transformation Demonstration Program
New York asked CMS to defer consideration of the serious mental illness (SMI) component of its IMD Transformation Demonstration Program amendment request until a later time to provide additional time for the State to consider meeting required implementation milestones under the SMI framework. New York also continues to engage with CMS about the flexibility to provide services to individuals who reside in a state mental health hospital or IMD for more than 60 days.
Coverage for Justice Involved Populations
New York and CMS continue to review the State’s request for limited coverage of specific services furnished to certain incarcerated individuals for up to 90 days immediately prior to the beneficiary’s expected date of release. CMS has approved this provision in California and Washington, and issued guidance encouraging states to pursue this option, and has released guidance for states for designing 1115 waivers to cover select services for justice-involved populations. Arizona, Illinois, Kentucky, and Massachusetts also have pending 1115 waivers to provide services to individuals prior to release from incarceration.
Continuous Eligibility for Children
The approved waiver highlights the State’s intent to submit an amendment to its demonstration in early 2024 to provide continuous Medicaid eligibility to children up to age six. CMS has approved this provision in Oregon, Washington, and New Mexico, and several other states have waivers with this provision pending or are seeking public comment from stakeholders on the provision.
Waiver Financing
Designated state health programs (DSHP) can be a key component of waiver financing, and states are required to put up the non-federal share of funding to “draw down” the federal Medicaid matching funds. In part, New York relies on DSHP to fund its non-federal share expenditures. CMS authorizes New York to claim up to $3.981 billion in total computable expenditures for DSHP; at New York’s 50% federal Medicaid match rate, this frees up nearly $2 billion in state funds to finance the waiver. Waiver initiatives cannot be exclusively financed by DSHP, and the State is required to contribute at least $351 million in non-federal share for the waiver period.
Looking Ahead
As NYS shifts to implementation of the waiver amendment, further critical details will come in the form of state program guidance and protocols that the State must submit to CMS, including:
- Submitting HRSN services and infrastructure protocols
- Initiating its application for the CMMI Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model and secure Letters of Intent from hospitals expressing interest in participating in the Model or another global payment model
- Analysis of current Medicaid provider payment levels to meet rate increase requirements for primary care, behavioral health, and obstetrical care.
Conclusion
CMS’s approval of New York’s 1115 waiver request highlights the agency’s continued support of state investments in HRSN, health equity, and efforts to support providers serving Medicaid members. The landmark investment in HRSN services for Medicaid members and use of a statewide health equity organization tied to regional SCNs will be closely watched as other states develop their own HRSN and health equity strategies to improve whole-person care.
NOTE: Full details New York State’s Health Equity 1115 Waiver Amendment are available through Manatt on Health, Manatt’s legal and health policy subscription service covering the topics and trends that are transforming health care. For more information, contact Barret Jefferds.
1 New York’s existing “Medicaid Redesign Team” waiver authorizes the State’s mandatory Medicaid managed care program, among other initiatives, and is in effect from April 1, 2022, through March 31, 2027.
2 CMS has applied the term “health related social needs” in its Medicaid policy framework for addressing social determinants or drivers of health. CMS clarifies that, “while ‘social determinants of health’ is a broad term that relates to the health of all people, HRSN relates more specifically to an individual’s adverse conditions reflecting needs that are unmet and contribute to poor health.”
3 New York submitted its 1115 IMD amendment request to CMS on December 21, 2022.
4 In its 1115 waiver amendment request, New York sought $6.7B in funding for financial incentives to Medicaid managed care plans and providers that meet State-set criteria for health-equity focused VBP contracts, with some structured as global prepayment arrangements.


